
The Standard American Diet (SAD) is a term used to describe the macro and micronutrient composition of the food Americans eat. It’s based on a consensus of mainstream nutrition experts drawing on data from the National Health and Nutrition Examination Survey (NHANES). [1]
The NHANES is an ongoing national study that surveys participating Americans about their diets.
According to the 2017-2018 NHANES data, the average American adult eats:

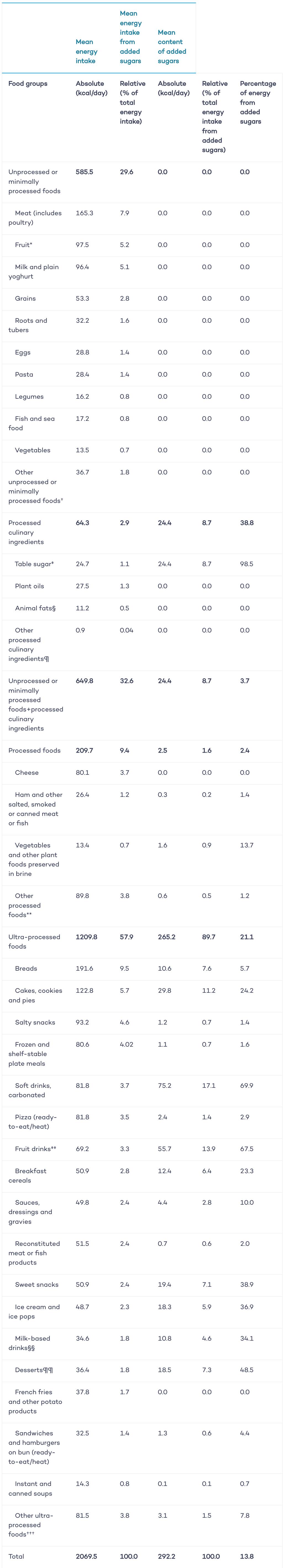
And according to a 2016 study in the BMJ journals, Americans get 58% of all calories from ultra-processed foods. [2]
The following graph shows the distribution of the total energy intake along with the energy intake from added sugars according to food groups, and the content of added sugars in each food group.
Younger Americans (from age 2 to 19) eat less protein (14%) and more carbohydrate (52%). [3]
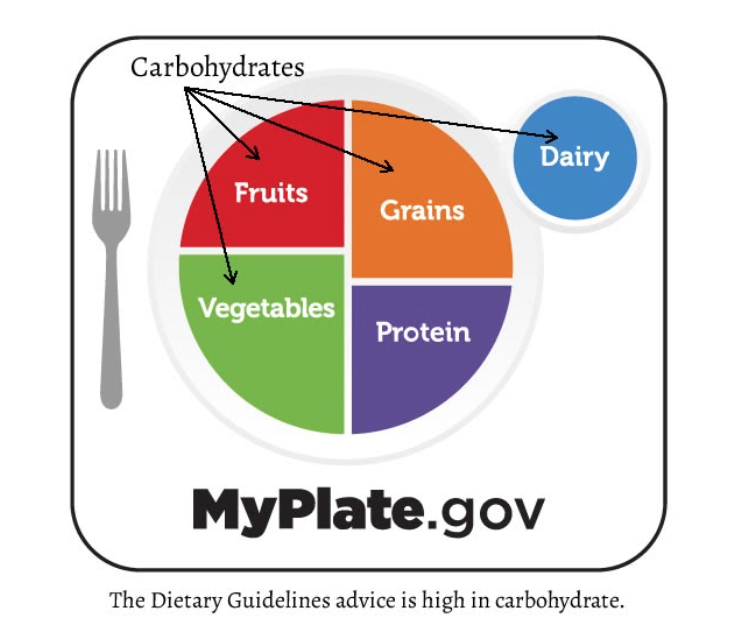
In addition, the federal Dietary Guidelines Advisory Committee analyzes the NHANES data and current nutritional research and creates the Dietary Guidelines for Americans (DGA).
The overall goal of the DGA is to advise people on what to eat to promote good health and prevent disease. This is where the USDA Food Pyramid comes from, and the more recent MyPlate graphic. These guides are supposed to positively influence the Standard American Diet.
The first DGA was released in 1980 and it gets updated every five years. The current 2020-2025 version hasn’t changed much. It still advises Americans to eat less fat and more carbohydrates for good health, despite a great deal of research that contradicts that advice. [4]
The DGA sets the ideals for what is healthy eating and then compares those ideals to the Standard American Diet.
The DGA says that Americans should eat fresh fruits and vegetables, whole grains, lean protein and healthy oils for good health.
When the SAD is compared to this ideal, the DGA says we eat too much-saturated fat in the form of red meat and high-fat dairy products, too much fast food, and too many refined carbohydrates, added sugars, salt, and overall calories. [5]
These less than ideal choices, they report, are why so many Americans suffer from the chronic diseases of obesity, heart disease, diabetes and cancer. As we shall see, some of these DGA charges are supported in scientific evidence, but not all.
For instance, relying on fast food for most meals does increase calorie, salt, and sugar intakes substantially, while reducing vitamin and mineral intakes needed for good health. This is especially true for younger Americans. [6]
However, the research shows that only about 37% of adults eat fast food regularly. In fact, as shown by the USDA Healthy Eating Index, a measure of diet quality, American adults make “healthy” food choices about 60-65% of the time. [7]
That means for a majority of meals, Americans follow the Dietary Guidelines. Yet, the problem of chronic diseases in the US continues to worsen. Let’s explore why this is the case.

The Nutrition Coalition, a respected group of dietary professionals, identifies the answer for the increase of chronic disease in America as rooted in the DGA’s recommendation to eat less fat and more carbohydrates.
They contend that the Dietary Committee has ignored research clearly indicating that too much dietary carbohydrate is the main cause for the current health problems plaguing Americans.
They recommend that a low-carbohydrate diet would be healthier for the American population, especially when considering that 60 percent of Americans already suffer from metabolic disorders. [8] Metabolic disorders refer to disruptions in the normal processes of breaking down food into its nutrient parts–fat, protein, sugar, vitamins, and minerals. High intake of carbohydrates is a primary factor for many of these disorders.
Interestingly, recent research published on the safety and health effects of low-carbohydrate diets strongly supports this conclusion. [9] [10] [11]
Yet the DGA Committee chose to largely ignore these studies as they debated the 2015 and the 2020 Guideline publications. The current MyPlate graphic shows that the DGA still recommends most Americans get most of their calories from plant-based carbohydrates.
To their credit, the DGA Committee did finally admit the low-fat diet they had been pushing for years was not supported scientifically. They also relaxed their recommendations for consuming less cholesterol. And they admitted that there was “no appreciable relationship” between dietary cholesterol and blood cholesterol levels.
In an article for the New York Times, Nina Teicholz, the director of the Nutrition Coalition writes “Americans, it seems, had needlessly been avoiding egg yolks, liver and shellfish for decades.” [12] Teicholz’s concern over how the DGA “experts” got our dietary advice wrong for so long calls into question the current DGA’s advice.
When we look at the origins of SAD, we see that it is a modern aberration in the human race’s dietary history. For millions of years, mankind ate almost no carbohydrates. [13] It’s only in the recent past that we have made carbs the center of our daily meals.
The modern human (homo sapiens) race, according to science’s best guess, evolved into being about 200,000 years ago. But our ancient ancestors were walking the earth much earlier.
The first humanoid animals depended on a plant-based diet and had brains no larger than a chimpanzee. At about 2.5 million years ago, Paleolithic man learned to scavenge meat from other predator kills. With the addition of that nutritionally-dense food, human brains and digestive systems began to change. [14]
Over the next few million years, our ancestors developed tools that helped them become true hunters, and as the amount of meat they consumed increased, brain size and cognitive ability expanded.
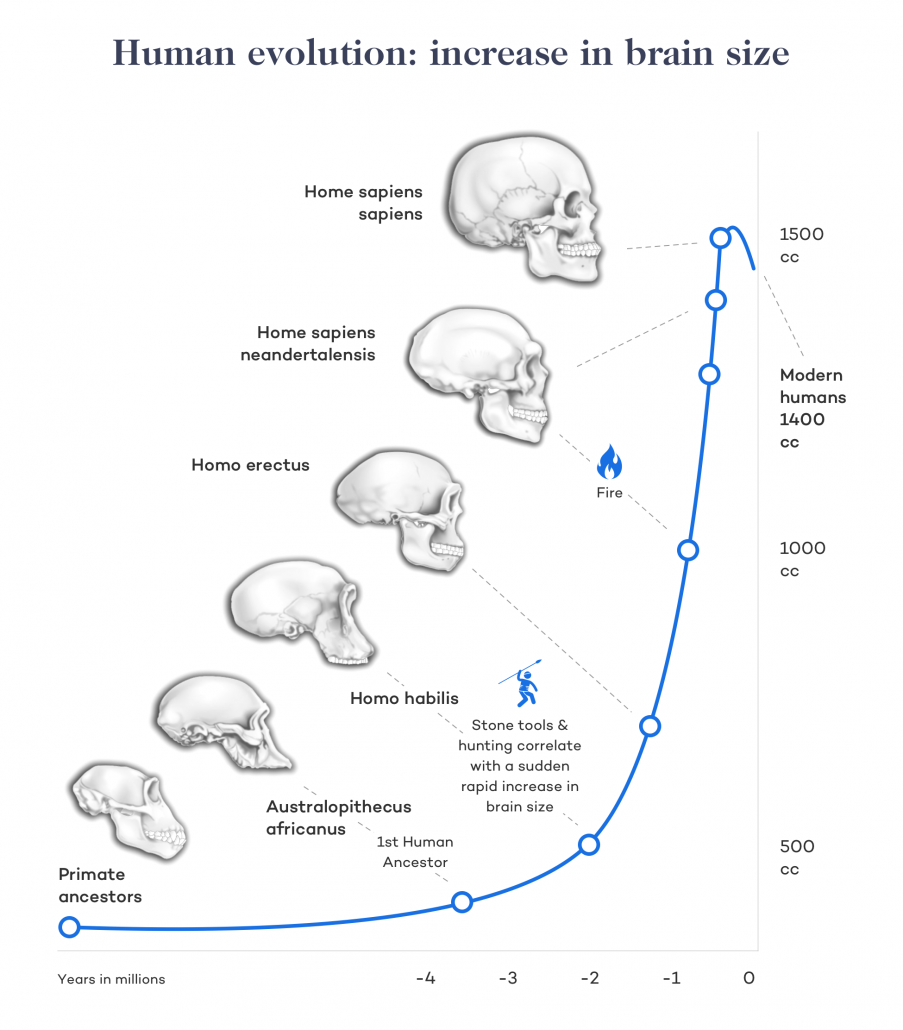
Around 100,000 years ago, humans had learned to throw a spear with speed and accuracy and to catch and cook seafood. That meat-rich diet, high in nutritional resources for brain growth, resulted in the human ability to speak and think abstractly, trade with others, create art and clothes, and migrate across continents to find more food and better places to live.
Then, around 10,000 BC, modern humans learned to farm. And that’s when our collective human health started to decline. [15] This shift from hunting to agriculture is the not so ancient origin of the SAD.
After only a few thousand years of agriculture, (between 8000-3000 BC) much of the human population had stopped wandering after wild animal herds and started settling into life as Neolithic farmers. We began domesticating animals and growing and eating cereal grains such as wheat and corn.
As ancient humans began to consume more cereal grains and less meat, bone health and resistance to disease began to deteriorate.
Studies of early Neolithic human remains show that by 3000 BC, farmers were several inches shorter than hunter-gatherers and their bones and teeth show evidence of mineral disorders such as rickets and osteoporosis.
There were also indications of severe vitamin and mineral deficiencies and a proliferation of infectious diseases. In addition, evidence indicates infant mortality rates were high, and the average span of a farmer’s life was shorter too. [16]
And so here we are. After more than two million years of a diet rich in animal protein and fat, modern humans switched to eating cereal grains in an evolutionary microsecond.
And in the last nanosecond of 200 years, we added refined carbohydrates and industrial oils to our diets.
Unfortunately for us, our genetic adaptation process works on a million-year time frame, so our genetic profile is pretty much the same as it was 200,000 years ago. Hence, we are experiencing the collective health costs of eating a diet we are not genetically equipped to handle. This is quite clear if we look at the current health data and note the prevalence of the “diseases of civilization”.

The phrase “diseases of civilization” refers to how in first-world, wealthy countries, the manner in which people eat and live causes them to die from chronic diseases such as diabetes, cancer, inflammatory conditions and heart disease.
Much of the current research supports the assertion that refined carbohydrate consumption is the main culprit in the proliferation of these disease states, in large part because high blood sugar increases body inflammation, which triggers other disease processes. More on this later.
Inflammation is a condition in which a person’s immune system has been triggered to fight some sort of irritation or damage taking place within their body.
For example, an immune system response is what causes the pain and redness around the area of a splinter in one’s finger. If the offending cause is not removed, the immune system response and the associated inflammation itself can eventually become a chronic condition which causes further damage.
Chronic inflammation is implicated in a wide variety of diseases including heart disease, metabolic syndrome, and diabetes, cancer, autoimmune conditions such as rheumatoid arthritis, infertility, and mental disorders such as depression. [17] [18]
One of the main triggers for chronic inflammation in the body is rampant glycation. This is a process where the sugar molecules in the bloodstream stick to our cells and tissues.
A small amount of glycation is normal and can easily be repaired by the body. But when a person’s daily diet includes large amounts of carbohydrates, blood sugars become chronically high, glycation rates increase, and a chain reaction of damage is set off that results in increased inflammation. [19]
The carb-fueled inflammatory process is one of the main factors linking the standard American diet to cardiovascular disease.
Cardiovascular disease is typically associated with damage to the body’s vascular system. This system of blood vessels brings oxygenated blood from the lungs to the heart and other body systems.
Consuming lots of refined carbohydrates sets up a domino effect in which glycation and inflammation injure the linings of the blood vessels supplying the heart. [20] [21] [22]
As inflammation sets into those injured areas, a loss of vessel suppleness leads to high blood pressure. Further injury leads to atherosclerosis (the infamous “hardening of the arteries”) and vascular blockages which can trigger a heart attack and stroke.[15]
The high carb intake of The Standard American Diet contributes to diabetes by spiking insulin levels and increasing Inflammation. Diabetes is one of the most damaging diseases of civilization. People with diabetes can no longer manage the amount of sugar in the bloodstream.
In 2018, the Centers for Disease Control (CDC) reported that more than 34 million Americans had diabetes. Type 2 diabetes is the most common by far and is strongly linked to refined and total carbohydrate consumption.[16] Both staples of the Standard American Diet.
The human body is not designed to handle consistently high amounts of sugar. Eating carbs for three meals a day with snacks in between floods the bloodstream in toxic levels of glucose. This constant stream of glucose stresses the adrenal glands and stimulates your pancreas to produce the hormone insulin in excessive amounts.
Over time, increased levels of blood sugar and insulin result in high levels of glycation and inflammation which trigger more widespread damage including:
The high carb intake of the standard American diet is also a factor in the development of cancer.
Many types of cancer cells rely on high blood sugar to flourish and grow. Consuming large amounts of carbohydrates provides the fuel they need. [23]
Inflammation is also a factor in tumor development and cancer metastasis. [24]
In short, eating a SAD diet high in refined carbohydrates sets up conditions in the body that encourage the establishment and growth of cancer.
An important point to note here is that the USDA Dietary Guidelines advise that red meat consumption should be limited because it is linked to cancer in many epidemiological studies.
However, a meta-analysis of the research on the relationship of red meat consumption to cancer mortality was published in 2019 and concluded that the “possible effects of red and processed meat consumption on cancer mortality and incidence are very small and the certainty of evidence is low to very low.” [25]
The carbohydrate-rich standard American diet is also strongly linked to inflammation within the intestinal system.
Case rates of chronic inflammatory bowel diseases have increased significantly since 2015, with over a million people in the United States suffering from either Crohn’s disease or ulcerative colitis. [26]
The intestinal tract is home to billions of gut bacteria collectively termed the gut microbiota.
This ecosystem of organisms helps us digest our food while protecting against foreign toxins. It’s also responsible for producing essential vitamins and neurotransmitters.
Recent research indicates that healthy gut microbiota is critically important not only to a properly functioning digestive system, but for our overall mental, metabolic, and nervous system health. [27]
The Standard American Diet afflicts the gut when sugar, fiber, and plant toxins damage cells lining the intestinal tract. The immune system responds to the damage with an inflammatory response that destroys gut bacteria. This allows the infiltration of toxic organisms, which encourages further inflammation.
Wheat gluten and other cereal grains and flours are major offenders in gut cell damage and inflammatory bowel conditions. Several studies report that foods high in fermentable carbohydrates (FODMAPS) worsen irritable bowel conditions. [28]
Although red meat consumption is often cited as a factor in bowel diseases, little controlled research data exists to support this hypothesis. At least one controlled study shows that reducing red meat intake does not reduce the rate of Crohn’s disease flare-ups. [29]
Another body system that’s sensitive to the high carbs and plant toxins in the Standard American Diet is the reproductive system.
Research confirms that high blood sugars can increase the amount of glycation and oxidative stress within the reproductive organs. This results in reduced ovarian function and dysfunction in the granulosa cells which protect egg development. [30]
High levels of glycation also reduce the activity of female steroid production and follicular development in the ovaries. [31] And finally, glycation and oxidative stress also cause damage to the capability of male testicles to produce normal sperm cells[25].
The standard American diet also causes an imbalance of essential fatty acids. You’ve probably heard the term omega-3 and omega-6 fatty acids during commercials for fish oil supplements. But what are these substances and why are they important in our diet?
Omega-3 and omega-6 essential fatty acids (EFA) are “essential” because they cannot be synthesized by the body and must be derived from dietary sources. They are also polyunsaturated, a term that refers to the types of chemical bonds within the molecules.
Fats like butter and coconut oil have stable chemical bonds called “saturated” bonds and so are called saturated fats. Olive oil has one unstable bond and is a monounsaturated fatty acid or MUFA. But omega-3 and omega-6 fatty acids have multiple unstable chemical bonds, so they fall in the category of polyunsaturated fatty acids or PUFA.
We only need a small amount of PUFA each day, but they are vitally important as they play a role in nearly every metabolic function in the body.[26] And each type of essential fatty acid has different effects on body systems, as shown in the graphic below.
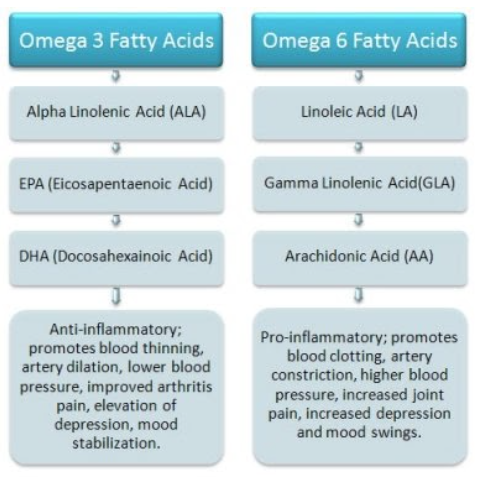
Essential fatty acids are also sources for the body’s production of a class of hormone-like molecules called eicosanoids.
These molecules are among the most potent regulators of cellular function, and they are produced by almost every cell in the body. Eicosanoids exert a wide-ranging and profound influence on your health. Among other important effects, they regulate blood pressure, lung function, and blood clotting mechanisms.
The type of eicosanoids that are dominant within the body depends on the types of essential fatty acids being consumed in the daily diet. In general, since omega-3 fatty acids have an anti-inflammatory effect on the body, eating more omega-3 rich foods results in an accumulation of anti-inflammatory eicosanoids. In contrast, eating more omega-6 fatty acids results in an increase of eicosanoids which have pro-inflammatory properties.
In the last 100 years, the amount of omega-3 polyunsaturated fats in the Western diet has declined while the consumption of omega-6 fatty acids has increased substantially. This is due to the development and use of vegetable and seed oils in our food supply.
The USDA advises Americans that vegetable and seed oils (olive oil, soybean oil, canola oil, and sunflower oil) are healthy fats, but it neglects to mention these oils are highly processed industrial products.
Not only are they high in inflammatory omega-6 fatty acids, but their production process introduces other toxins such as hexane and pesticides into the final product. [32] Almost all processed foods contain one or more vegetable oils.
The abundance of omega-6 oils in the standard American diet tilts it toward being pro-inflammatory, and not surprisingly, research links an imbalance of omega-3 to omega-6 fatty acids to a long list of chronic disease, including heart disease, cancer, diabetes, and other metabolic diseases [33] , pregnancy issues [34] and mood disorders such as depression and bipolar disorder. [35] [36]
The body of research on the relationship between mental health and diet continues to grow, and it supports the hypothesis that not only is a deficiency of anti-inflammatory fatty acids such as EPA[32] involved, but that oxidative stress[33] can be a trigger for mental issues as well.
Many psychiatric disorders can be linked to issues with the optimal amounts of brain neurotransmitters such as serotonin and dopamine. Julia Ross, MA is the author of a book called the Diet Cure, and she lays out the evidence for how blood sugar instability and fatty acid deficiencies can impair our brain chemistry. Other research points to the link between refined carbohydrate intake, gut health, and psychological disorders. [37] [38]
To improve our health, we now know that most Americans should avoid the high blood sugars, inflammation, gut microbiota damage, and fatty-acid imbalances characteristic of the consumption of too many carbohydrates and processed oils. So what do we eat instead?
A ketogenic, high-fat, low-carbohydrate diet fits the prescription nicely. It reduces not only refined but total carbohydrate intake. HFLC eating also encourages the consumption of healthy, natural fats and fresh meats and seafood. The result is a diet moderate in protein, low in carbohydrate, and rich in good fats.
The health benefits of a ketogenic diet include lower blood sugar and insulin levels, less glycation and inflammation, support for optimal brain function, and a reduction in the likelihood of developing or worsening heart disease, cancer or a metabolic disease such as diabetes. [39] [40]
For many Americans, the Standard American Diet’s reliance on carbohydrates, especially refined carbohydrates as our main source of calories does not promote good health.
The Standard American Diet increases body inflammation and triggers blood sugar and glycation issues that foster diseases such as heart disease, cancer, and diabetes.
In addition, relying on processed foods high in Omega-6 fatty acids upsets our essential fatty acid balance which can contribute to inflammation, and result in brain chemical derangement, mental health disorders.
Fortunately, we now have research to support the choice of a high-fat, low-carb diet to help us avoid or reverse many of these “diseases of civilization” and help us stay healthier for the duration of our lives.
Now we’re all waiting for the USDA Dietary Guidelines committee to get on board with the current research and provide the American public with science-based nutrition advice.

.png)
.png)
We’re a global community of seekers, healers, and doers committed to reclaiming health on our own terms. When you join the Kiltz Mighty Tribe (KMT), you’ll gain access to education, support, and collective wisdom.


